“The danger, for the species, is not going where it is going, but going there with eyes shut, with legs gone mad, and a drunk brain.”
George Duhamel, L’Humaniste et L’Automate (1933)
1. Digitalization: A New Determinant of Health
When pandemics sweep through societies they upend critical structures such as health systems and medical protocols, economic activity and patterns of behavior, socioeconomic classes and relations, ingrained institutional arrangements, and everyday community and family lives. In 1918-1919, three waves of the Spanish Flu not only had devastating demographic consequences (between 50 and 100 million deaths), but also caused deep social disruptions and created a climate of general mistrust that permanently affected individual behavior.
Covid-19, too, has caused unprecedented disruptions to healthcare, globally. This has played out on two fronts: the ‘direct’ effects the pandemic has had on countries’ healthcare infrastructures, and the ‘indirect’ effects that have resulted from states’ efforts to mitigate the crisis. While the immediate response of governments was to adopt extensive lockdowns and travel bans to flatten the curve of the viral contagion, mounting economic pressures and unmet population needs have since forced them to gradually reopen societies and economies while safeguarding public health, controlling the spread of the infection, and implementing safe-distancing measures. This balancing act has triggered the need for digital solutions and transformations in many sectors, enabling remote work and the continued provision of services while ensuring people’s safety and minimizing avoidable human contact.
This shift has pushed the health sector to seek out tools that had been met with resistance before the pandemic. In the United States, public health infrastructures had already been underfunded for decades, saddling the sector with outdated and clunky technologies. As Covid-19 swept across the country, it looked as if Big Tech’s analytical firepower and new focus on health emergencies could help overcome the dire healthcare problems and “save the world”. Healthcare systems had to reorganize service provisions for existing patients to reduce face-to-face (F2F) appointments, attend to triage cases that demanded urgent consultation, postpone non/less-urgent visits or surgeries, and set up new infection control measures. They also had to address the surge in patients who contracted Covid-19, including those with respiratory diseases, while minimizing their proximity with others receiving treatment for non-Covid illnesses. These changes required the reconfiguration of workflows and physical infrastructure to reduce the risk of healthcare-associated transmission. Digital technology and new models of care were deployed to meet these challenges. At the same time, the pandemic laid bare the consequences of the deep digital divide within and between high-and low-income countries; it demonstrated that many developing countries lacked the institutions and infrastructure to support health digitalization.
On the biomedical front, available capacities for data generation, sharing, and analysis boosted research efforts around SARS-CoV-2. Chinese scientists made the genetic code of the virus available to the global research community in one week, making the development of diagnostic tools possible in record time. South Korea managed to flatten the curve at an early stage of the outbreak through the deployment of artificial intelligence (AI) and the real-time polymerase chain reaction (RT-PCR) testing scheme. Large-scale digital data collection and coordinated trials have since helped develop a reasonable understanding of the viral kinetics and risk factors. Beyond the scope of biomedical research, the pandemic has accelerated the demand for digital technologies to advance and sustain broader public health objectives, both by expanding the use of existing tools (telemedicine) and deploying digital innovations (survey apps, contact-tracing applications, and compliance monitoring tools, including quarantine measures).
Yet, the pandemic has also revealed the downsides of digitalization. Efforts by governments to track the virus digitally has exposed the digital divide between and within countries, as well as the considerable differences that exist across jurisdictions on the degree of permissibility in data collection and processing. The necessity of digital technologies in the fight against Covid-19 should not draw attention away from the lopsided ways in which these tools have been adopted, often exacerbating pre-existing social inequalities. Oftentimes, health or health-related data derived from mobile apps and online interactions have been used not to trace contacts but rather to limit people’s movements and monitor societal compliance with emergency rules. These instances have made it clear that letting digital platforms and technologies go ungoverned sets the scene for “human rights black holes”. In order to avoid injuring the future of healthcare amid the ongoing technology rush, the scientific community must ask itself a few fundamental questions that go beyond issues surrounding Covid-19.
It has been pointed out that “the way we enable, administer, and check the exceptional surveillance and social powers that each government exerts to contain Covid-19, especially as implemented through technology systems, will frame an important part of the future of state power in a world with increasing emergencies”. The rapid advance of the pandemic has opened our eyes to the dire question of how to reconcile a democratic understanding of data privacy with the public health demands of disease control, surfacing the many ethical, societal, and human rights dilemmas that lie at the intersection between the private and public value of health and personal data.
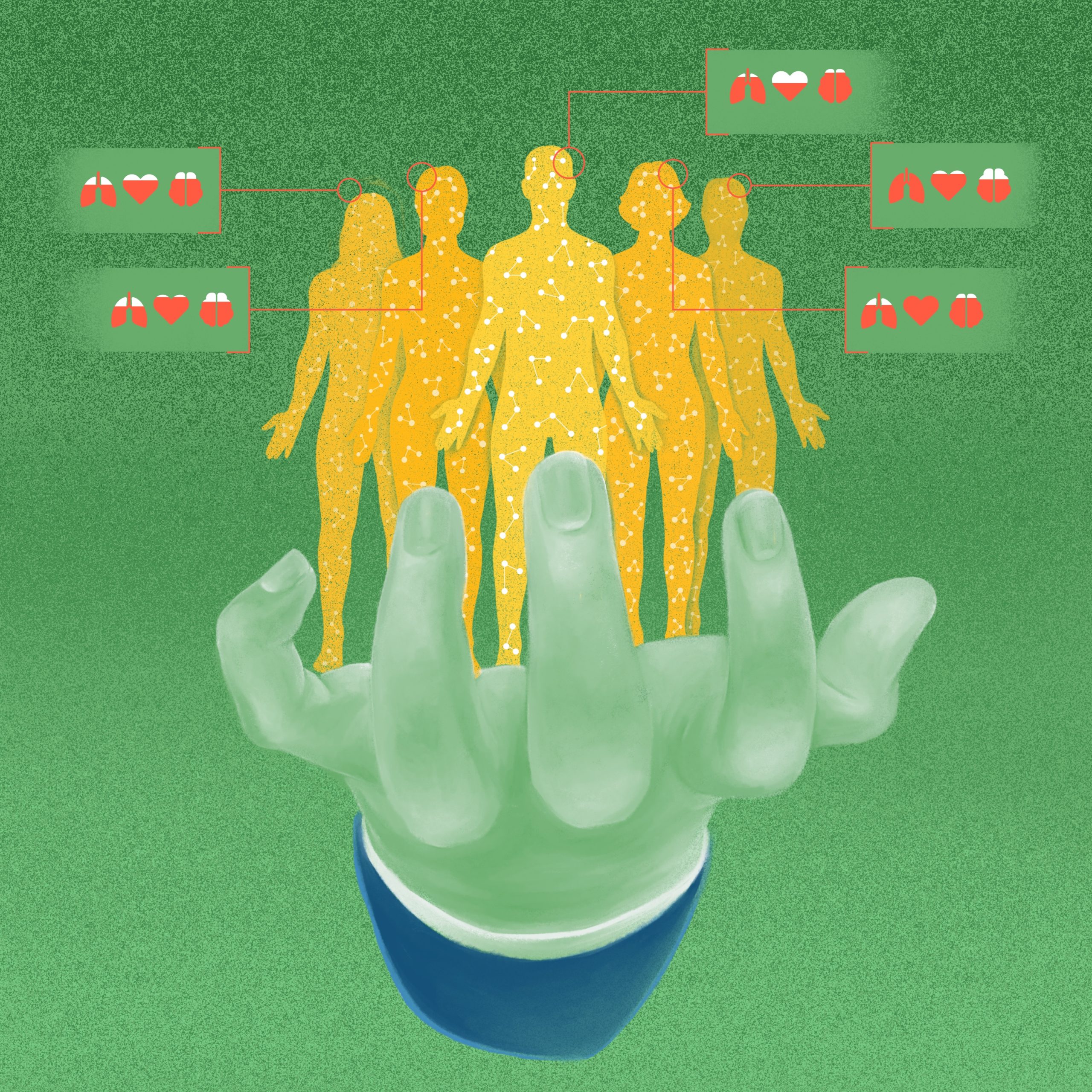
Looking retrospectively at the various disease-management approaches used during the pandemic, this essay attempts to examine ‘how’ value-based and participatory digital governance mechanisms could help reposition the (often) untouchable component of data protection in the event of future viral outbreaks for the sake of health rights. With digital technologies becoming an increasingly relevant health determinant, our thesis is that we need to build a governance architecture that generates trust in digital health, by empowering people and patients, while firmly regulating powerful Big Tech players. Established public health concepts enshrined in the World Health Organization’s (WHO) Health for All strategy are essential to guarantee that digital transformations advance social justice and promote equity. The realization of the right to health as the basis for all human rights, including the right to privacy, dignity, and non-discrimination, represents an unavoidable normative framework to orient the new scenario shaped by digital transformations.
2. Digital Health: The Penicillin of our Time?
Over the past few decades, the neoliberal reconfiguration of healthcare and global health governance in favor of market-driven approaches has paved the way for the digital health industry, eagerly pushed by the euphoria and techno-optimism associated with the “new economy” of the late 1990s. Amid the onslaught of geopolitical, financial, and public health crises, private-sector led technological fixes have garnered increasing political and societal salience. The data economy that has emerged in the process, now, intervenes in all aspects of human life. Well before Covid-19, the digital economy had penetrated the medical and paramedical fields through behavioral tracking, interpretative algorithms, and geo-localization, all geared towards the development of mobile health 1 Such is the case of Apple HealthKit, Google Fit, and Ibm Watson.and the transformation of medicine into a data-generating/data-driven practice. The embrace of policies that have promoted a unilateral distancing from public models of healthcare provision, and the push for datafication as the necessary response to emerging viruses and growing health threats, are examples of trends that have enhanced precision medicine and its controversial armamentarium, in a swirling kaleidoscope of progress, expectations, limitations,2Existing efforts to harness advances in genomic sequences to support precision medicine are hindered by a lack of diversity in genomic datasets, as genomic variants from areas with high genetic diversity, such as Africa, India, and other areas from the Global South, are significantly underrepresented when compared with European populations. and dilemmas. As the world transitions into an era of ‘life measurement’, computational systems increasingly modeled on the human brain have become the new frontier in healthcare, creeping out of their labs and guiding ‘real’ people to make ‘real’ life decisions. Their unflinching verdicts have led the rush to the emerging “economy of attention” — the most valuable asset of the digital age — and to the shaping of what has been labeled as the “industry of life”. In other words, people’s health needs are being managed by automated assistance to orient actions into a promised sphere of human wellness. This is the expanding space where facial expressions, voice, heartbeats, and gait become profitable sources of data to allow provision of the best personalized response through so-called “affective computing” or “emotion AI” that is said to recognize, express, and adapt to human emotions. As we will see, mental health is the pasture land for new herds to colonize.
Amid the onslaught of geopolitical, financial, and public health crises, private-sector led technological fixes have garnered increasing political and societal salience. Well before Covid-19, the digital economy had penetrated the medical and paramedical fields through behavioral tracking, interpretative algorithms, and geo-localization, all geared towards the development of mobile health and the transformation of medicine into a data-generating/data-driven practice.
In this ‘seamless economy’, which extends beyond health, math-powered applications have started to shape a quasi-umbilical bond between the individual and the digital company via the progressive intrusion of products into consumers’ lives. But the anthropomorphic transformation of AI capitalizes any minimum existential manifestation and transforms life’s psychological flows, its emotional states, and plurality of gestures into an endless source of economic power and financial wealth. It portends a new order of things based on maximum reactivity and return, to which all individuals and institutions need to adapt and respond, but its models are black boxes whose contents are fiercely-guarded corporate secrets.
The pandemic presents a historic opportunity for extending the multidimensional power of Big Tech players. According to Global Pandemic App Watch, by December 2020, at least 74 countries had launched apps to automate and support manual contact tracing, a key public health strategy for breaking the kinetic of contagion. Many governments resorted to smartphones to promote public health functions such as population surveillance, case identification, modeling and evaluation of interventions, and communication with the public. Smartphone apps, interconnected with a wider range of digital technologies, were used for syndromic surveillance, machine learning and natural language processing, and digital diagnostic and genomics. The “smartphone pandemic” has thus considerably expanded the capacity of governments to discipline ‘individual’ behavior, as observed in the 2020 Freedom House report and in Singapore’s management of the virus. Under pressure of the health emergency, citizens have become “ever more visible to their governments, but not the other way round”, as the UN Special Rapporteur on extreme poverty and human rights had presciently warned in 2019. With Covid-19 continuing to resurge in phases, this “state of exception” has advanced unrestrained. While the global technological industry “remains virtually a human rights-free zone”, its power and domination have been increasingly employed to guide, restrict, or incentivize individual actions. Only a handful of critical scholars have highlighted that those digital tools are not neutral and risk deepening existing discriminations and inequalities based on class, ethnic identity, gender, and age. Some have also pointed to the public health and health equity implications of Big Tech for low-and middle-income countries already dealing with major health system challenges.
3. Big Tech: Too Big, Too Unbridled?
While lockdowns and tangled supply chains weighed on the retail, service, and industry sectors, Silicon Valley superpowers, such as Alphabet, Apple, Microsoft, Meta, and Amazon, used the pandemic to report record profits. In April 2021, their combined revenue rose by 25% to over USD 1.2 trillion as compared to the prior year, making Big Tech CEOs unbelievably rich amid the devastation wrought by the pandemic. Apple accumulated so much extra cash that it spent an additional USD 90 billion, nearly the equivalent of Kenya’s gross domestic product, to purchase its own stock.
The rapid pace of Big Tech’s advancement has invaded the health economy which, in a post-pandemic context, interacts ever more with the digital one. In the United States, venture capital funding for digital health companies has soared, with 2020 witnessing funding worth USD 14.1 billion, a 72% increase from 2018. The global market for AI-driven healthcare is expected to reach USD 34 billion by 2025, with a potential value of USD 300 billion created by 2030. These projections don’t fully capture the Covid-19 effect.
Big Tech players have also moved further into each other’s turf during the pandemic. Market dynamics have shifted from direct competition to controversial business strategies, including a faster pace of mergers and acquisitions in the wake of the health emergency. The reliance of most governments on a few huge companies for key technological infrastructure has undermined their public digital sovereignty. By now, it is evident that no country could set up an effective contact-tracing app without the cooperation of Apple and Google, whose operating systems power 99% of the world’s smartphones. The alliance between tech giants and governments triggered by the pandemic, especially on contact tracing, epidemic modeling, and public health communication, was justified by the assumption that private companies would rescue unprepared and underfunded health systems with their analytical firepower. Most such success stories have emerged from Asian countries, where digital solutions have been used as one element of a more comprehensive and well-functioning public health strategy for pandemic preparedness and response. African countries have also experimented with digital approaches, but at the cost of private corporations exploiting their weak regulatory framework. These countries, overall, have been far less able to integrate the digital response within the public health system, thereby benefiting private healthcare. The power asymmetries of the technological ecosystem have certainly undermined the agency of national governments and their ability to leverage digital transformations in the interest of their people’s health.
From the perspective of the political and legal determinants of health, pandemic alliances between Big Tech and states “differ from formalized public-private partnerships that have been scrutinized within the global health literature, in that they are more ad hoc, informal, and opaque forms of engagement with little, if any, public accountability”, Storeng highlights. Both wield intrusive powers with inconsistent regard for privacy and human rights. 3https://www.stopspying.org/snooping Both share a not-so-humble awareness that they can orient public behavior. Analysts have predicted that enhanced partnership during the pandemic, often grounded in experimental solutions, may end up creating a power apparatus with far greater imperialistic tendencies than the one resulting from the 9/11 attacks. There is a lot that the digital response to Covid-19 reveals about the current reconfiguration of the balance between public responsibility and corporate power that is skewed to benefit the latter. This is especially concerning when it comes to setting global health priorities and strategies. Every day, Facebook and Google survey millions of people all over the world: not even the United Nations has the ability to do that.
Beware of “Emotion AI” Amid reports of staggering increases in mental illnesses, Covid-19 has exacerbated the need for therapists, and particularly the growth of affecting computing 4 There are sensory wristbands that can monitor one’s sweat, skin temperature, and blood flow, and through a connected app ask users to select how they are feeling from a series of predefined labels (“content”, “distressed”, etc.). Companion Mx is a mobile app that examines users’ voices to detect signs of anxiety. Conversational agents such as Woebot Health use emotion AI to adapt the principles of cognitive behavioral therapy to treat depression and provide advice on sleep, and stress-sentiment analysis applied in chatbots combines sophisticated natural language processing (NLP) and machine learning techniques to determine emotions expressed by the users. therapeutics. Tracking people’s emotions is a natural next step in the digital intrusion in our lives. “Emotion AI” is a field of computer science working to build technology that can predict and model human emotions for clinical application. Affecting computing is forecast to become a USD 37 billion industry by 2026. It has emerged as an attractive approach for governments and corporations to address the swelling trends of the mental health crisis disproportionately affecting children and young adults, among other exposed, underrepresented, and underserved population groups.
Of course, AI requires a simplification of psychological models and neurobiological theories on the functions of emotions. Emotion AI cannot capture the diversity of human emotional experience — voice inflections and gestures vary from one population to another — and the need to quantify qualitative relationships is problematic: emotions are no hard science. It also risks being embedded with the programmers’ own cultural bias, a lack of objectivity that slides into racial bias. But, while digital companies popularize self-tracking applications that passively monitor data-fied lives, these technologies colonize wider populations without clinical oversight or human expert support, and in the absence of policies dictating who has the right to people’s ‘emotion data’ and what constitutes breaches of privacy. Changes in regulations to serve patients and protect healthcare workers has instead enhanced operational flexibility for psychiatric disorders and general wellness.5 In April 2020, the U.S. FDA announced it would expedite approval for digital solutions that offer services to persons suffering from depression, anxiety, obsessive-compulsive disorders, and insomnia. Developers would no longer have to state the different AI-ML-based techniques that powered their systems. By failing to provide instructions on the collection and management of emotions and mental-health sensitive data, the FDA announcement clearly demonstrated its neglect of patients’ privacy and data security. Depression detection by workplace software monitoring or wearables may cost individuals their sources of employment or lead to higher insurance premiums. BetterHelp and Talkspace, two counseling apps that connect users to licensed therapists, were found to disclose sensitive information with third parties about mental history, sexual orientation, and suicidal thoughts.
The post-Covid mental crisis is prospectively becoming a very profitable business venture: more than 20,000 apps dealing with mental health are now available to smartphone users. However, only 2.08% of them are supported by published, peer-reviewed evidence of efficacy. Also, these apps are labeled as “wellness products” in the United States, which exempts designing companies from the Health Insurance Portability and Accountability Act.
4. Data Privacy and Health Rights: Striking a Difficult Balance During Covid-19
Before the arrival of Covid-19, Big Tech was facing a “techlash” following a series of scandals around fake news and interference in democratic electoral processes which led to bad press and stricter regulations. With the onset of the pandemic, some hailed the demise of anti-Big Tech hysteria, while others speculated that issues like privacy and competition would no longer be pressing concerns, and that both consumers and regulators would develop a new appreciation for the value that the digital industry could bring to society. After all, tech giants had seized the momentum at the inception of the crisis to show their willingness to help fight the contagion, pledging USD 1.25 billion for SARS-CoV-2-related relief efforts.
But with the peak of the emergency wearing off, the moment of respite may have come to an end. If the early phase of the pandemic loosened regulatory oversight over healthcare solutions championed by the digital industry, its aftermath has placed greater scrutiny on tech power. Digital companies have become lifelines for many, but are still unable to resolve problems that occur at a massive scale. Besides, they have proven to be unreliable. Facebook failed to protect users from the spread of Covid-related health misinformation. Amazon had to grapple with massive underreporting of infections contracted in its warehouses and Zoom struggled with security flaws. Regulating the sector became a key concern for governments, including in response to the varying degrees of public acceptance/refusal of technology to fight the virus.
China was not the only country to clarify its relations with national tech titans and shift from toleration to confrontation through the launch of Operation Cyber Sword in October 2020. In the same month, the U.S. Congress released the results of a 16-month investigation to examine the state of competition of digital markets and the adequacy of existing antitrust laws, and U.S. President Joe Biden appointed vocal tech critics to lead antitrust agencies. A round of Big Tech regulations have been adopted across democratic setups, and in March 2022, Europe finally reached a landmark agreement on the Digital Market Act (DMA), a new chapter in antitrust enforcement for the digital economy. In the healthcare domain, companies that act as gatekeepers in the life sciences and digital therapeutics sectors will have to abide by new diligence obligations and transparency requirements in the way products are digitally marketed and advertised. This is especially relevant in areas relating to Big Data, the creation of digital tools designed to support research and better patient care. The management of personal data sourced from a core platform falls under the remit of Article 5(a) which “prohibits combining personal data sourced from a core platform service with data from other services offered by the gatekeeper or from third-party services”.
The pandemic has indeed raised questions regarding the choice between public health safety and data privacy. As the exponential rise in Covid-19 cases due to chain infections made manual tracing methods insufficient, the relevance of digital contact tracing came to light, and apps quickly unfolded in countries. How individual governments chose to organize digital tracing brought to light differences in regulatory strategies on data collection and management. The criteria for announcing a national health predicament and the implementation of crisis regulations is closely linked to a country’s own experiences of national emergencies, be it public health, economy, or war. Asian countries, for example, have benefitted from previous experiences with SARS. Their willingness to share data, or the mandated sharing of data to fight infectious diseases spelled out in existing or new laws, were grounded on these precedents. In Europe, on the other hand, past experience of fascist totalitarian rule through the declaration of emergency decrees and governmental control of private citizens’ lives has created a wariness about allowing the government access to personal data, even under a health plight. This widespread reluctance was deepened by the global surveillance revelations of the Snowden affair and by the Facebook-Cambridge Analytica scandal, which had stirred anger in Europe. The Snowden case had also eroded the American public’s confidence in the government collecting and processing data of its citizens. The discourse on protecting citizens’ personal information was largely fixated around the notion of civil liberties ‘in the free world’ against big government/capital powers, a narrative that has surfaced in multiple tropes, from the public protests on mandated mask-wearing guidelines and forced closures and lockdowns, to the domain of vaccine politics. Moreover, what the European and the American public lacked before the onset of Covid-19 was the experience of mass deaths from infectious diseases.
The pandemic has indeed raised questions regarding the choice between public health safety and data privacy. As the exponential rise in Covid-19 cases due to chain infections made manual tracing methods insufficient, the relevance of digital contact tracing came to light, and apps quickly unfolded in countries.
Covid-19 Management: The South Korean Way
South Korea’s heavy reliance on automation and AI during the Covid-19 pandemic was the result of the country’s investment in internet and digital infrastructure over the past two decades. What is often underplayed in South Korea’s early pandemic governance is the role of Big Data analysis involving AI and the legal grounds of its implementation, whereby lessons from another coronavirus outbreak — the Middle East Respiratory Syndrome (MERS) in 2015 — led to the rapid design and deployment of the Covid-19 “Triple T” strategy (testing/tracking/treating). The need for digital contact tracing also prompted a review of the Infectious Disease Control and Prevention Act (IDCPA), providing the legal grounds for health authorities to access citizens’ personal data on a conditional and temporary basis through a centralized and mandatory electronic tracking system. South Korea’s Personal Information Protection Act (PIPA) was enacted in tandem with the comprehensive implementation of IDCPA to offset the negative consequences of the invasion of personal privacy, if and when such instances should occur in pandemic governance efforts. While technology and culture helped in terms of responsible citizenship, the role of civil society in Covid-19 containment has been assessed as a key contributing factor, since the government has always acted as a coordinator of multiple partners in the country at the national and local levels.
The Covid-19 Smart Management System (SMS) was launched in March 2020, enabled by the smart city data hub platform that had been set up years before SARS-CoV-2 to conduct Big Data analyses of energy, transportation, environment, and safety in cities by the Ministry of Land, Infrastructure and Transportation (MOLIT). South Korea’s SMS was indigenously developed with no concerns about the market position of Google and Apple as providers of smartphone operating systems. To ensure accuracy and speed in the epidemiological survey, the system was designed as a cooperative inter-organizational network, with the Korean National Police Agency, the Credit and Finance Association, three telecom companies, and 22 credit card companies granted access to infection data within the SMS portal, through global positioning system (GPS) tracking. Other mechanisms that entailed use of GPS data, such as the apps for self-quarantine and self-diagnosis operating on a mandatory basis upon border entry, were deployed by the Ministry of Interior and Safety and the Korea Disease Control and Prevention Agency (KDCA). The fact that South Korea’s conditional collection and use of personal data (deleted after 14 days) was promoted by public demand to bring the Covid-19 emergency situation under control, and based on a purposeful revision of the social contract enshrined in national legislations, has been obscured by outside observers. On the contrary, these observers have blamed South Korea’s history of authoritarianism for its legalization of conditional data collection during Covid-19.
The European Union’s strong advocacy for the General Data Protection Regulation (GDPR) as the standard legal foundation for digital data collection and use implied that protection of users’ data privacy was one of the core elements of developing contact-tracing apps. With the GDPR forbidding the collection and use of data, digital app downloads and usage relied entirely on citizens’ will. In April 2020, the first pan-European dialogue to develop a common Covid-19 app failed, and EU countries opted to launch their own national apps, in a departure from initial ideas of centralization.6Germany had advocated for a centralized standard called Pan-European Privacy Preserving Proximity Tracing (PEPP-PT) with the support of a coalition of European scientists and digital technologists. If the PEPP-PT had been implemented, with its “privacy-preserving” standard that does not require the collection of location data, it would have required Google and Apple to make changes to the decentralized application programming interface (API) that they were designing. Initial discussions at the EU-level were held in April 2020, envisioning a pan-EU app for all EU countries. But the conversations quickly fell through and countries chose to take their own paths to adopt decentralized apps, with striking variations in downloads and societal receptions. The collaboration between Google and Apple to come up with an application programming interface (API) further boosted the leverage these two tech giants could exert on decision-making with regards to deployment of digital tools for public policy purposes. 7Despite the mounting health emergency, Google and Apple did not want to change their operation system settings for the centralized apps to work. This refusal proved to be a crucial stumbling block in the negotiation between tech companies and national governments trying to launch a Covid-19 tracing app on mobile phones. However, once the Google-Apple API was provided as open source, countries delegated the task of app development to private companies in their jurisdictions, or to public tech organizations within the bureaucracy. This meant not only that the quality of each national app varied significantly across EU member states and U.S. states, but also that interoperability was considerably jeopardized, as exposure notifications were not possible when citizens traveled across EU or U.S. states. In Europe, this approach has not necessarily reflected a positive use of technology in the prevention and containment of the viral disease. Recognizing this shortcoming, the Council of Europe proposed a draft legislation to revise the GDPR and, after several consultations, the European Commission, in May 2022, announced a new Regulation of the European Parliament and of the Council on the European Health Data Space that takes stock of Covid-19 lessons.
After the huge boost Big Tech companies received during the pandemic in the form of increasing market share and expanding wealth, regulating the sector may not be easy. The power asymmetries of the new digital ecosystem have undermined the agency of many national governments and their capacity to pursue digital transformation processes in the best interest of their people’s health. Legislations risk becoming outdated before they are even enacted. One risk is that the recent wave of policy initiatives may problematically trigger new sophisticated forms of enforcement bailouts and self-regulations — a slippery scenario given governments’ dependency on digital technologies for the functioning of their societies. Besides, in the absence of a common framework and direction, issues arising out of digitalization cannot be addressed with old rules. The risk is that even if economies recover after Covid-19, neither competitors nor regulators may be able to dampen the position that Big Tech reached during the pandemic.
After the huge boost Big Tech companies received during the pandemic in the form of increasing market share and expanding wealth, regulating the sector may not be easy. The power asymmetries of the new digital ecosystem have undermined the agency of many national governments and their capacity to pursue digital transformation processes in the best interest of their people’s health.
5. Concerns and Opportunities for the Future
As the medical Internet of Things (IoT) becomes the new normal for an increasing number of people in the world, the growing symbiosis between tech companies and governments during the pandemic has elicited heated debates and reactions against the excesses of technology-driven solutions to the public health crisis, especially on issues of data management, privacy, efficacy, discrimination, and exclusion. The low download rates of contact-tracing apps in Europe is a solid indicator of shaky confidence turning into fearful disenchantment. The growing alliances between these and other influential actors in the health field — health insurers, doctors’ networks, etc. — may, in the future, promote further privatization of health services and normalize health data infrastructures built on the principle of large-scale data collection and exchange. Defined in almost every country by operational vulnerability and lack of preparedness, irrespective of the degree of economic development, the health crisis may have menacingly provided an opportunity to accelerate new ecosystems across industrial sectors (digital, pharmaceutical, financial, etc.). It has allowed corporate actors to impose their vision, strengthen market control, further influence healthcare research and policy agendas, manipulate multilateral decisions, and shape the scenarios for future pandemics.
Mounting concerns about intelligence capitalism as a totalizing force in a divided multilateral scene mark a turning point in civic awareness and mobilization.8Such is the case of Accountable Tech, Privacy International, Main Street Against Big Tech, or in the field of health research: see in this regard The Digital Health and Rights: Participatory Action Research Project by the Graduate Institute, among others.This awareness is good news, because it leads to more critical analysis and literature, and sets the conditions for new digital scenarios as the urgent agenda for action. Key disclosures from within the digital world have greatly helped in this regard. The battle for tech, clearly, matters. Yet, despite the exponential growth of digital health and health data, this remains a particularly sensitive and fragile domain for mobilization due to a combination of factors. Firstly, the corporate capture of global health civil society organizations (CSOs) during Covid-19, especially through philanthropic foundations’ interventions, has oriented the provision of funding towards technological support in the fight against the pandemic. 9Amazon and Google have provided tailored packages of financial support to NGOs and community organizations during Covid-19 through their non-profit initiatives. This has prompted an uncritical acceptance of the indispensability of private tech giants in tackling global health challenges. Besides, the global health community has long dismissed the impact of digital ecosystems on health rights. Instead, it has hailed health digitalization as the solution to the widespread fragility of healthcare infrastructures, and embraced it as a quick fix that can fill structural gaps and improve vulnerable populations’ health conditions. Global health CSOs have undervalued and grossly delayed a political conceptualization of the faultlines and key questions underlying new digital transformations. Will digital technologies increase the availability and acceptability of quality health services? Will they change the nature and direction of healthcare through the use of wearables and AI applications, Big Data and genomic technologies, and online consultations with health professionals? Will digital transformations enfranchise patients and communities by correcting their (mostly) hierarchical relationship with health professionals and providers, thus shaping health systems according to peoples’ needs?
Following Covid-19, multinational technology behemoths have embedded themselves deeper within countries’ health systems. It will, therefore, be harder than ever to disentangle them from being an integral component of the health service architecture. The current practices of data extraction risk concentrating financial and political/legal power in the hands of companies that hold massive amounts of data and technical capacity in order to extract value from them. But if properly governed, the increased availability and use of health data could facilitate more timely and transparent decision-making, as well as communication to health system managers and policymakers. We argue that any tensions between health and digital transformations should be resolved in favor of the core values of health and the WHO’s Health for All approach — namely, distributive justice, democracy, solidarity, equity, and individual and collective human rights — while also (re)interpreting such principles to exemplify their relevance in a digital world. Upholding these values serves to ensure that digital technologies enable health benefits and advance health data solidarity as part of a new social contract. For this to happen, it is imperative to put in place a new global mechanism for binding multilateral consensus on digital governance. The humanist ideals of the Health for All paradigm cannot be manipulated to dress up and continue promoting the ruthless digital ecosystem emboldened by finance capital that systematically subverts them. That’s why we need to confront the current norm-setting for the digital space which is increasingly shifting to post-democratic plurilateral spaces (such as the OECD Committee on Digital Economy) and/or to private sector-driven rule-making through centers of power such as the World Economic Forum (WEF), which operate through new tropes of digital colonization.
Any tensions between health and digital transformations should be resolved in favor of the core values of health and the WHO’s Health for All approach — namely, distributive justice, democracy, solidarity, equity, and individual and collective human rights — while also (re)interpreting such principles to exemplify their relevance in a digital world.
When it comes to health, the articulation of governance frameworks that lie at the intersections of technology and global public policy needs to start with a clear distinction between public interest and private interests in data use. This can be done through:
- the creation of an international taxonomy of health data that can be used to diversify the level of protection and the norms governing their use;
- the definition of international standards for health data interoperability through open and collaborative approaches;
- the framing of agreed rules for the sharing of health data and health-related data, with the aim to achieve the cross-border dimension of data solidarity, namely, the timely and transparent sharing of data during public health emergencies, such as pandemics.
Social activism and enhanced digital mobilization are crucial to steer this agenda after three pandemic years, and particularly now that Russia’s invasion of Ukraine may have permanently upended how internet companies operate. This momentum cannot be lost. CSOs will have to keep pace with digital technological advancement and foster an integrated culture around Big Tech’s unaccountable digital power. Across constituencies, and well beyond the issue of privacy, CSOs will need to engage in a relentless campaign to dismantle Big Tech totalitarianism, and advocate for global health justice and people-centric development reframed for the digital age. Being part of a digital justice movement must be an aspiration and priority for those who aim to protect health rights in the coming years. The global health community must act to make a strategic dent on the multistakeholder governance model that has given rise to and shaped digitalization, and that is increasingly designing the futures of health.